What Is a Genotype and Why Does It Matter?
Your genotype represents your complete genetic makeup, containing all the hereditary information that determines everything from your eye color to your susceptibility to certain diseases. When it comes to blood-related conditions like sickle cell disease (SCD), understanding your genotype becomes particularly crucial for making informed decisions about family planning.
The major hemoglobin genotypes that impact sickle cell disease risk include:
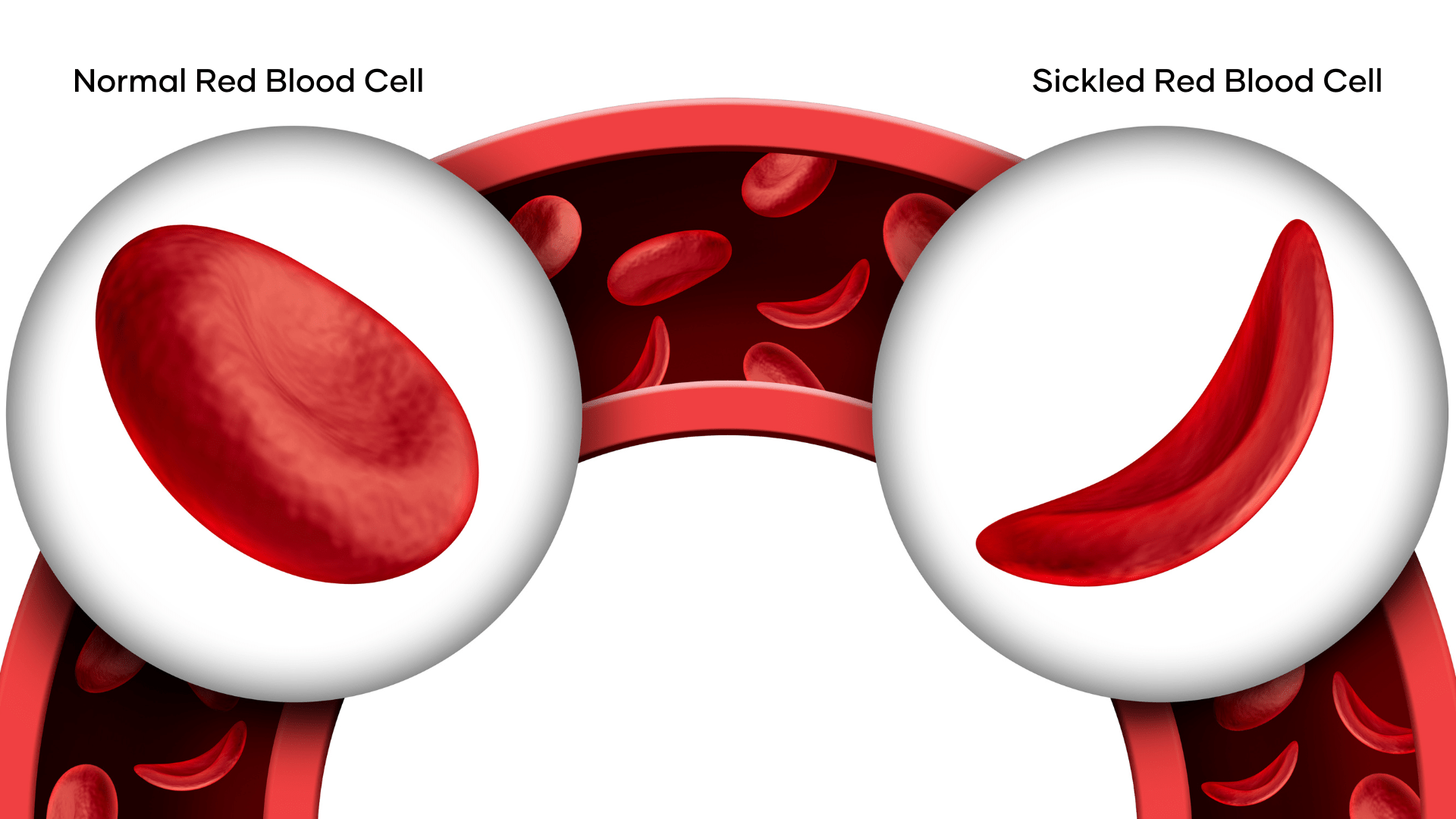
- AA Genotype: Normal hemoglobin structure with no sickle cell trait or disease. Individuals with this genotype have completely healthy red blood cells that efficiently transport oxygen throughout the body.
- AS Genotype: Carrier status of the sickle cell trait. These individuals typically don’t experience symptoms but can pass the trait to their children. Under extreme conditions such as severe dehydration or high altitudes, mild symptoms may occasionally occur.
- SS Genotype: Indicates sickle cell disease, a serious genetic blood disorder that causes red blood cells to become rigid and sickle-shaped, blocking blood flow and causing numerous health complications.
- AC Genotype: Carrier of hemoglobin C, which is generally asymptomatic but can cause mild anemia in some cases.
- SC Genotype: A form of sickle cell disease that combines hemoglobin S and hemoglobin C, typically resulting in a moderately severe condition.
- Other Variants: Include genotypes like SD, SE, and SOArab, each with their unique implications for blood health and overall wellbeing.
AS/AS Genotype Combination
Sickle cell disease follows an autosomal recessive inheritance pattern, meaning a child must inherit two copies of the abnormal gene (one from each parent) to develop the disease. Understanding this pattern is essential for prospective parents, particularly those with the AS genotype.
When two individuals with the AS genotype have children, the probability of different outcomes per pregnancy is as follows:
- 25% chance (1 in 4) of having an AA child (healthy, non-carrier).
- 50% chance (2 in 4) of having an AS child (a carrier like the parents but generally healthy).
- 25% chance (1 in 4) of having an SS child (sickle cell disease, which can lead to lifelong health challenges).
Every pregnancy carries a 1 in 4 risk of producing a child with sickle cell disease (SS), a severe genetic condition that affects red blood cells and can lead to chronic pain, infections, organ damage, and reduced life expectancy.
The Reality of Living with Sickle Cell Disease
Children born with sickle cell disease (SS genotype) face numerous challenges that affect their quality of life and development. Understanding these challenges is crucial for prospective parents considering their family planning options.
- Pain Crises
Sickle cell pain crises, also called vaso-occlusive crises, occur when sickled red blood cells block blood vessels, preventing oxygen from reaching tissues. These episodes can be excruciating, requiring hospitalization and potent pain medication. Triggers often include dehydration, extreme temperature changes, physical overexertion, stress, infections
- Increased Vulnerability to Infections
Children with sickle cell disease have compromised immune function, particularly related to the spleen. This vital organ, which helps fight certain infections, often becomes damaged early in life. As a result, these children face higher risks of potentially life-threatening infections including Pneumonia, Meningitis, Septicemia (blood infections), Osteomyelitis (bone infections)
Preventive measures typically include daily antibiotic prophylaxis, regular vaccinations, and prompt medical attention at the first sign of fever.
- Growth and Development Challenges
The chronic oxygen shortage caused by sickle cell disease can significantly impact a child’s physical development:
- Delayed growth milestones
- Below-average height and weight
- Puberty that begins later than peers
- Delayed sexual maturation
These issues can affect self-esteem and social development during crucial formative years.
- Long-term Organ Damage
Over time, the sickling process damages multiple organ systems:
- Splenic Sequestration: The spleen can trap red blood cells, leading to rapid enlargement and potential life-threatening anemia
- Acute Chest Syndrome: A severe lung injury that causes chest pain, fever, and breathing difficulty
- Stroke: Children with sickle cell disease have a significantly higher risk of stroke due to blocked blood vessels in the brain
- Eye Damage: Progressive vision problems, including blindness, can result from retinal vessel damage
- Kidney Dysfunction: Reduced filtering capacity can lead to protein loss, concentrating problems, and eventual kidney failure
- Heart Complications: The heart must work harder to pump blood, potentially leading to heart enlargement and heart failure
- Avascular Necrosis: Bone death, particularly in the hip and shoulder joints, due to compromised blood supply
- Quality of Life Impact
Beyond physical symptoms, sickle cell disease significantly affects daily life:
- Frequent school absences due to illness and hospitalizations
- Limitations on physical activities and sports participation
- Psychological challenges including depression and anxiety
- Social isolation due to chronic illness
- Financial strain on families due to medical expenses
- Career limitations and employment challenges in adulthood
- Life Expectancy Considerations
While medical advances have dramatically improved survival rates, individuals with sickle cell disease still face a reduced life expectancy. In developed countries with access to comprehensive care, many people with sickle cell disease now live into their 40s, 50s, and beyond. However, complications can still lead to premature death, particularly in regions with limited healthcare resources.
Family Planning Options for AS/AS Couples
Couples where both partners have the AS genotype have several options to consider when planning their families. Medical advancements have created multiple pathways to parenthood that can reduce or eliminate the risk of having a child with sickle cell disease.
1. Comprehensive Genetic Counseling
Genetic counseling provides personalized guidance for couples facing genetic risks. A qualified genetic counselor can:
- Explain inheritance patterns in easy-to-understand terms
- Help couples process the emotional aspects of their genetic risk
- Outline all available reproductive options
- Connect couples with support groups and resources
- Guide decision-making based on personal values, religious beliefs, and cultural considerations
Many healthcare providers recommend genetic counseling before conception for couples with known genetic risks.
2. Prenatal Testing Options
For couples who conceive naturally, prenatal testing can determine if the developing fetus has sickle cell disease.
Chorionic Villus Sampling (CVS): Performed between 10-13 weeks of pregnancy. It involves collecting a small sample of placental tissue. The results typically available within 2 weeks and carries a small risk of miscarriage (approximately 1%)
Amniocentesis: Performed between 15-20 weeks of pregnancy. It involves collecting amniotic fluid surrounding the baby. The results are typically available within 2 weeks and slightly lower risk of miscarriage than CVS (less than 1%)
Non-Invasive Prenatal Testing (NIPT): While traditional NIPT cannot yet reliably detect sickle cell disease, research in this area is progressing rapidly. This blood test analyzes fetal DNA in the maternal bloodstream and may soon provide a risk-free alternative to invasive testing for sickle cell disease.
After receiving prenatal test results, couples can make informed decisions about continuing the pregnancy, preparing for a child with special healthcare needs, or in some cases, considering pregnancy termination where legally available and aligned with personal values.
3. Advanced Reproductive Technologies
In Vitro Fertilization (IVF) with Preimplantation Genetic Testing (PGT): This cutting-edge approach allows couples to have biological children without sickle cell disease:
- Ovarian stimulation to produce multiple eggs
- Egg retrieval and fertilization with partner’s sperm in a laboratory
- Embryo development to the blastocyst stage (5-6 days)
- Removal of a few cells from each embryo for genetic testing
- Analysis to determine which embryos have AA or AS genotypes (no sickle cell disease)
- Transfer of selected healthy embryos to the uterus
- Cryopreservation (freezing) of additional healthy embryos for future use
While this approach virtually eliminates the risk of having a child with sickle cell disease, considerations include:
- Cost: IVF with PGT is expensive, typically ranging from $15,000-$30,000 per cycle
- Success Rates: Pregnancy is not guaranteed, and multiple cycles may be needed
- Insurance Coverage: Many insurance plans do not cover these procedures
- Emotional Toll: The process can be physically and emotionally demanding
- Ethical Considerations: Some couples may have concerns about embryo selection and disposition
4. Alternative Family Building Options
Some AS/AS couples choose to build their families through non-biological means:
Adoption: Adoption provides a pathway to parenthood while eliminating genetic risks. The adoption process varies widely in terms of wait times, costs, and requirements, but resources are available to guide prospective adoptive parents through each step. Options include:
- Domestic infant adoption
- Foster care adoption
- International adoption
- Relative adoption
Donor Gametes: Using donor sperm from an AA genotype donor can eliminate the risk of sickle cell disease when the female partner has the AS genotype. Similarly, egg donation can be considered when the male partner has the AS genotype.
How to Make Informed Choices for Family Planning
- AA + AS: Results in 50% AA children and 50% AS children. No risk of sickle cell disease.
- AA + AA: Results in 100% AA children. No risk of sickle cell trait or disease.
- AS + AC: Low risk of serious conditions, though SC children may have moderate complications.

Understanding your genotype and its implications is empowering. With advances in genetic testing, counseling, and reproductive technologies, couples have more options than ever before to make informed decisions about family planning.
For AS/AS couples specifically, knowledge is the foundation for navigating the complex decision-making process. By understanding risks, exploring options, and accessing appropriate resources, these couples can pursue their dreams of parenthood while making choices aligned with their personal values and circumstances.
Whether choosing natural conception, assisted reproductive technologies, adoption, or other family-building paths, the key is making decisions based on complete information and comprehensive support.