So, you’ve probably heard about the pills, the ring, the shot, and the implant, and it honestly sounds like a bad movie series you forgot to binge.
Or maybe you’re already on hormonal birth control and your doctor mentioned something about progestin and oestrogen. You smiled and nodded like you understood, but deep down, you’re thinking, “What is going on?”
We get it, and we’ve got you covered. Whether you’re trying to avoid pregnancy, tame your period cramps, or you’re just a curious bee about hormonal birth control and all the hype (or fear), this article is for you!
We’ll cover the types of hormonal birth control, their pros, cons, and how to figure out which one might work for you and your lifestyle.
What are Hormones, Really?
Hormones are tiny, powerful chemical messengers that regulate everything in your body. In terms of your reproductive system, the VIPs involved are:
- Oestrogen: helps build the lining of your womb.
- Follicle-Stimulating Hormone (FSH): helps mature the eggs in the ovaries.
- Progesterone: helps stabilise your womb lining and prepares for a little bun in the oven.
- Luteinizing Hormone (LH): helps trigger ovulation (egg release).
These hormones rise and drop at different points during your menstrual cycle, and influence when you see your period and ovulate. You can read more about the phases of the menstrual cycle here!
What Is Hormonal Birth Control?
Hormonal birth control options are methods that use synthetic versions of hormones – oestrogen, progestin, or both. They are like fake but fabulous versions of your body’s natural hormones.
Depending on the method, they can work in one, two, or all of these three ways by:
- Preventing ovulation: They can shut down the party before it even begins. No egg = nothing for the sperm to fertilise.
- Thickening your cervical mucus: This makes it nearly impossible for the sperm to swim through. Imagine trying to swim quickly in a pool full of honey. It’s not exactly the same, but it’s a visual guide.
- Thinning the lining of your womb: If an egg somehow manages to get fertilised against all odds, the thinner lining makes it harder to implant, like trying to plant a seed on concrete.
How Does Hormonal Birth Control Really Work?
Here’s the plot twist: if you’re on hormonal birth control, that monthly “period” you see isn’t a real period! Shocker, we know!
The reason is that hormonal birth control methods are little tricksters. They keep your body exposed to a steady level of oestrogen and/or progesterone, and your brain, being a trusting queen that she is, falls for it and thinks ovulation has already happened (spoiler: it didn’t).
Your brain then doesn’t bother to release FSH and LH, the hormones that help with ovulation. No FSH = No egg matures. No LH = No egg release.
Since ovulation didn’t actually happen, your womb lining doesn’t build up like it normally would, and since there’s barely any lining, there’s not much to bleed.
The monthly period that you see, if you see it, is actually called a withdrawal bleed. This happens when you take a break from the active hormones in your birth control, e.g. during the placebo week of the pill. Since there are no active hormones, that nice steady level drops, and your body goes, “Oh, no hormones? Let’s shed…something”. So, it sheds the thin lining.
It feels like a period. Looks like a period. But, in medicalese, it is not a real period from a real menstrual cycle.
What Are the Types of Hormonal Birth Control?
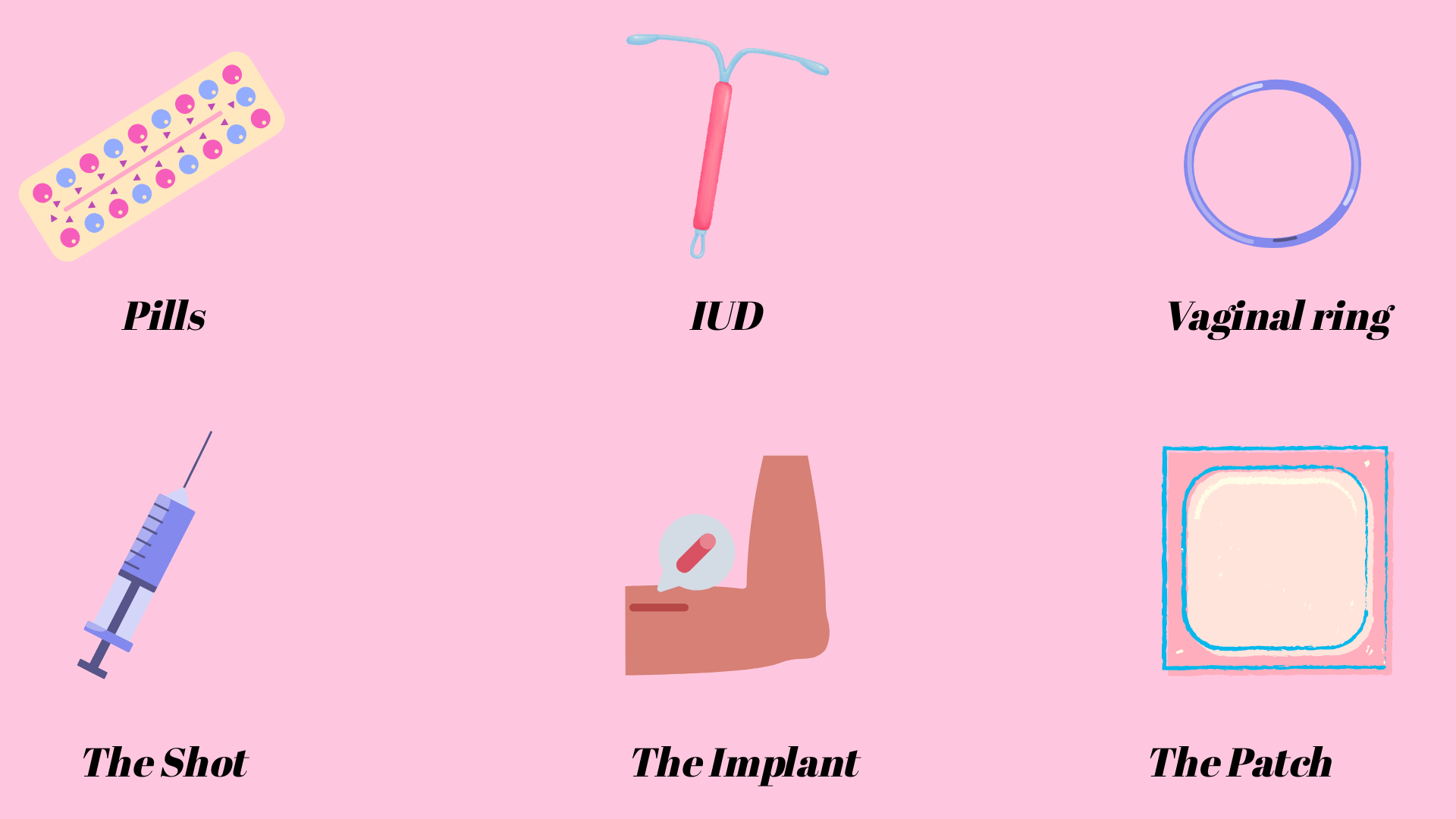
1. The Combined Pill
What it is: Also known as Combined Oral Contraceptives (COCPs), as they contain both oestrogen and progestin. There are 28 pills: 21 hormone-packed pills and 7 placebo pills.
Effectiveness: When taken perfectly, it is about 99% effective. But life happens, and so with typical use (missing a pill here and there, etc), it is about 91% effective.
Pros:
- It can make your “periods” lighter and regular, reduce menstrual cramps, and improve acne.
- It can reduce your risk of ovarian and endometrial cancers.
Cons:
- You have to take it daily and at the same time (no skipping!), which is not ideal if your schedule is all over the place.
- Side effects like sore boobs, headaches, nausea, mood changes, or spotting between periods can occur in the first few months.
- It contains oestrogen, so it is a no-go for people with migraines with aura.
- There is also an increased risk of blood clots, especially in women who are older than 35 and smoke, or have a family history or personal history of clotting disorders (side eye oestrogen!).
2. The Mini-Pill
What it is: It’s a solo act, so it contains just progestin. It can suppress ovulation, but not as consistently as COCPs. There’s no withdrawal bleed, so no “period”
Effectiveness: It is 99% effective with perfect use and 91% effective with typical use.
Pros:
- Safe while breastfeeding.
- A go-to for people who can’t use oestrogen, like those with clotting disorders or with certain migraines.
Cons:
- Must be taken same time every day (give or take 3 hours).
- Although there’s no withdrawal monthly bleed, there are still chances of irregular bleeding or spotting.
- May cause headaches, sore breasts, and mood changes.
3. The Patch
What it is: It’s a small sticker-like patch you wear on your skin. It contains both oestrogen and progestin. It is changed once a week for 3 weeks and not worn on week 4, so the withdrawal bleed happens.
Effectiveness: It’s about 99% effective with perfect use and 91% with typical use.
Pros:
- You only need to change it once a week. So, less fuss than the pills.
- It can also help with acne.
Cons:
- It can cause skin irritation.
- If the patch falls off or isn’t changed on time, the protection drops.
- It may not be as effective in people with higher body weight.
- The side effects are also similar to the pills – mood changes, breast tenderness, or spotting.
4. The Shot (e.g., Depo-Provera)
What it is: It’s a hormone injection that contains progestin, which you get every 12 weeks.
Effectiveness: It is about 99% with perfect use. With missed shots, it is about 94% effective.
Pros:
- Take it just 4 times a year. No daily or weekly stress.
- Many experience lighter periods after a year.
Cons:
- Irregular bleeding or spotting in the initial months
- It can cause delayed return to fertility (could take 6 to 12 months after your last shot).
- The side effects may include weight gain, mood changes, headaches, or bone thinning (with long-term use).
5. The Vaginal Ring
What it is: It looks like a small clear flexible bracelet, but for your vagina. You insert it for 3 weeks, then remove it for 1 week (withdrawal bleed). It contains oestrogen and progestin.
Effectiveness: It is about 99% with perfect use and 94% with typical use.
Pros: It is changed once a month, so less daily hassle.
Cons:
- Some women find the insertion uncomfortable.
- If it is not done properly, slips out, or stays in for too long, then protection can be reduced, and pregnancy can occur.
- The side effects are similar to the pill.
6. The Implant (e.g., Nexplanon)
What it is: It is a tiny rod, kind of like the size of a matchstick, that releases progestin. It is placed under the skin of your arm by a trained doctor.
Effectiveness: Over 99% effective.
Pros:
- Long-lasting, up to 3 years.
- Set-it and forget-it style, so no daily or monthly upkeep is needed.
Cons:
- It may cause spotting, which typically improves after 6 to 12 months,
- Irregular bleeds or no bleeds at all
- Other side effects may include mood changes or sore breasts.
7. The Hormonal Intrauterine Device (IUD)
What it is: A small T-shaped device inserted into your womb by your doctor. It contains progestin.
Effectiveness: Over 99% effective.
Pros:
- Very low-maintenance vibes. It can last from 3 to 8 years, depending on the type.
- Can reduce or stop periods.
Cons:
- Insertion may be uncomfortable or painful.
- Some people may experience spotting, which typically improves after 6 to 12 months, while others may stop getting their periods.
- In the very rare chance that pregnancy occurs, it may lead to an ectopic pregnancy (rare risk).
How to Choose the Right Hormonal Birth Control
Here’s a quick cheat sheet based on your vibe:
- Hate remembering pills/can’t be bothered? Consider the implant, shot, or hormonal IUD.
- Have migraines with aura or a high risk of clots? Avoid oestrogen and choose progestin only (mini-pill, shot, implant, or hormonal IUD).
- Taking other meds? Some drugs like rifampin (for tuberculosis), certain seizure drugs, and even St. John’s Wort can make most hormonal birth control less effective. The hormonal IUD usually stays effective regardless, but you should talk to your doctor about backup methods like condoms.
- Want fertility back ASAP after stopping? Ditch the shot. Try the pill, patch, or ring.
- Dealing with heavy periods, PCOS, endometriosis, or acne? Combined methods (oestrogen and progestin) can help with symptom relief. Some progestin-only options, like hormonal IUD, can also help, especially if you’re avoiding oestrogen.
- Worried about weight gain? Avoid the shot, because it has been linked to actual weight gain in some users.
The real tea on weight gain: Most studies state that the pills, patch, or shot don’t cause true/significant weight gain. However, some people report water retention or bloating, especially in the beginning. Individual experiences may vary, so if your jeans feel tighter, it’s not just in your head.
Final Thoughts
Hormonal birth control methods can be a lot, but they come with their perks as well.
If you’re not sure which to choose, have a quick chat with our doctors to help you find your perfect match.
Up next in this series: The non-hormonal birth control crew, from copper IUD to condoms to permanent methods and everything in between.
References
Hormonal Methods of Contraception – Women’s Health Issues – MSD Manual Consumer Version
Appendix D: Classifications for Combined Hormonal Contraceptives