Trying to choose the right birth control can leave you drowning in an endless sea of confusion. There’s a whole lot going on, from those you swallow to those you insert, or even the ones you inject.
Then there’s the important matter of side effects and failure rates, and figuring out what your body actually likes. Why does it feel like you need a PhD just to figure out which method works for you?
Whether you’re trying to avoid pregnancy, manage your hormones, or just want to be in control, you deserve to make the right choice. Not for your family member, not for your friend who swears by “just drink salt water after sex”(spoiler alert, it doesn’t work), but for YOU.
Let’s help make this decision simpler. In this birth control series, we’ll be discussing the different birth control methods, their effectiveness, and how to choose the best option for yourself. This article is your go-to starting point for figuring out the basics and what birth control options are out there.
Quick Myth Buster
Let’s bust some myths real quick about some of the wildest things people swear work to prevent pregnancy.
“You can’t get pregnant if you pee right after.”
- Urinating after sex is great for preventing UTIs. Babies, not so much?
“If you do it standing, you definitely wouldn’t get pregnant.”
- Sperm are determined little swimmers. Gravity wouldn’t save you from having a baby (or even 2 at once).
“You can’t get pregnant on your first time.”
- As long as there is an egg and a sperm, your chances of pregnancy are high, even if it’s your first time.
“Don’t worry. As long as he doesn’t cum, withdrawal method is effective.”
- Worry! Pre-ejaculate (aka pre-cum) can contain sperm. No matter how strong your partner claims his pull-out game is, there’s a real risk of pregnancy.
Now that we’ve cleared the air, let’s dive into what actually works, according to science!
What Is Birth Control?
Birth control (aka contraception) is any method used to prevent pregnancy. That’s the basic gist of it, but it’s more than just popping a pill or using a condom.
What Are the Types of Birth Control?
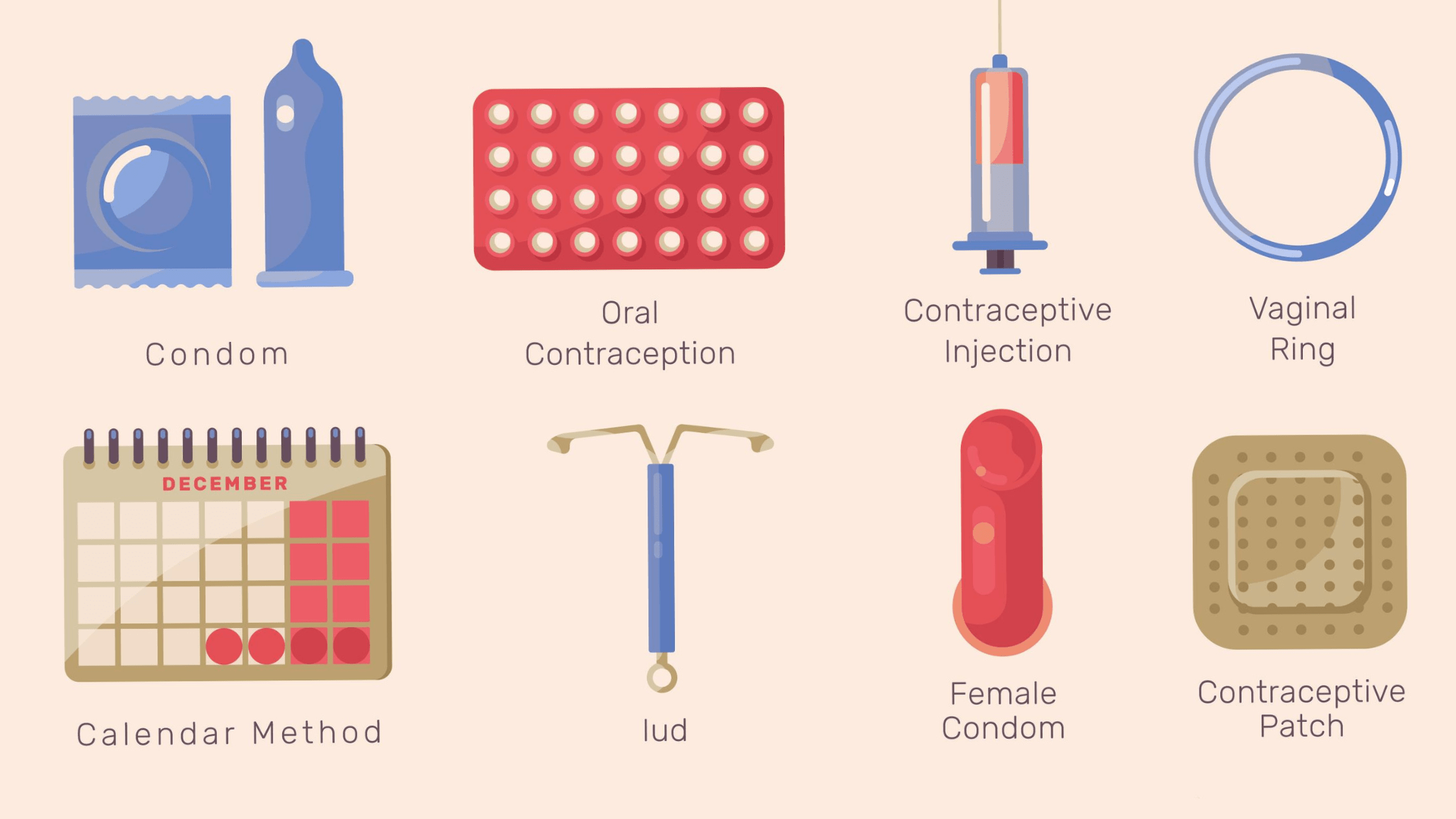
Here’s a quick overview of the birth control methods grouped into major categories:
Hormonal Birth Control
These use synthetic hormones (usually oestrogen/progestin) to either prevent ovulation (so the egg doesn’t mature and leave its nest), thicken the cervical mucus (so the very determined swimmers, the sperm, have a hard time getting to the egg), or thin the lining of the womb (so that even if the egg and sperm meet, there’s no cozy home for it). The different types of hormonal birth control include:
- The Pills: Taken daily. Some can also help with acne, cramps, and regulating your “period”.
- The Patch: Like a band-aid, but changed weekly.
- The Shot: Taken as an injection once every 12 weeks.
- The Implant: A tiny rod that is placed under your skin, and can last for 3 to 5 years.
- The Vaginal Ring: A flexible ring inserted in your vagina for 3 weeks, removed for 1 week, and then inserted again.
- The Hormonal Intrauterine Device (IUD): A small T-shaped device that is inserted into your womb and can last for 3-8 years, depending on the type.
They are effective methods, but each has its side effects, like mood changes, weight changes, or spotting (more on this in our next blog post).
Non-Hormonal Methods
If you want to ditch the hormones, your options include:
- Copper IUD: Hormone-free version of IUDs. It can last up to 10 years, but it can also cause heavy and more painful periods in the first few months.
- Barrier methods: This includes condoms (male, and yes, female ones), which can protect against both pregnancy and STIs. They also include diaphragms and cervical caps that cover the cervix, and spermicide, which is a chemical in gel, cream, or suppository form that kills sperm, and is usually used with other barrier methods.
- Fertility Awareness Methods (FAMs): This involves tracking your cycle and avoiding sex on fertile days.
Permanent Methods
For those who are sure they don’t ever want kids, or for the “I’m done with kids” gang, your options include:
- Tubal ligation or salpingectomy (for women): Tying or removing your fallopian tubes so the egg and sperm don’t have a meeting spot.
- Vasectomy (for men): Cuts the vas deferens (the tube that carries the sperm), which prevents the sperm from getting into the semen.
Emergency Contraception
This is used after unprotected sex or if your method fails (like a condom breaking). The options include:
- Levonorgestrel (e.g., Postinor): Works best within 72 hours.
- Ulipristal Acetate (e.g., Ella): Works best within 120 hours/
- Copper IUD: Can also work as emergency contraception if inserted within 5 days.
These are not for regular use, but they’re a solid plan B.
What Are the Benefits of Birth Control?
Birth control can be useful in preventing pregnancy, especially if you’re not trying to add “parent” to your million responsibilities at the moment. However, people also use it for other reasons, including:
- To regulate periods and ease cramps: Hormonal methods like the pill can be a game-changer if you’re dealing with irregular periods or period pain that has you feeling like your womb is against you.
- Reduce acne: Some birth control pills can help you get back to your “flawless, I woke up like this” era.
- Help with hormonal conditions: Birth control is often the treatment plan for people dealing with conditions like Polycystic Ovarian Syndrome (PCOS), endometriosis, and fibroids. It’s not a cure, but it can help with managing the symptoms.
How to Choose the Right Birth Control Method for You
There’s no one-size-fits-all for birth control, and the right option depends on your goals, your health, and even your daily routine. Here are some things to consider before making a choice:
What are your pregnancy plans?
- If you’re a short-term baby avoider, consider condoms, pill, patches, or the vaginal ring.
- If long-term, but you want reversible options, think IUDs or implants.
- If you’re very sure you don’t want kids in the future, consider the permanent options.
How good are you with routines?
- If you’re the organised girlie, with the daily reminder alarms and apps, the pills might work for you.
- If you want low-maintenance, consider the shots, implants, or IUDs.
Do you have other health conditions?
- If you have conditions like migraines with aura, blood clotting disorders, breast or endometrial cancers, or a history of stroke, oestrogen-based products like the combined pill, patch, and ring might not be safe.
- If you’re on some medications for seizures or tuberculosis, they can mess with some hormonal birth control methods and make them less effective.
What side effects can you live with?
- If you want to avoid mood changes or weight gain, then consider skipping some hormonal methods.
- If your vagina is a drama queen and gets easily sensitive, using vaginal rings, cervical caps, or spermicides might not be for you.
Do you want protection from STIs?
- If yes, then condoms are your go-to.
Final Thoughts
Choosing the right birth control is deeply personal. Our bodies are beautifully different, and we all have different needs. So, whether you’re into the tiny rods, the pills, or just good ol’ condoms, your choice should depend on what your needs are.
If you’d like to go over your options with a doctor, your Fertitude besties have your back. You can speak with a doctor here to help make an informed and personalised choice.
In our next blog post on this series, we will break down hormonal birth control, the pros, the cons, and all the drama involved.
References
Birth Control – Clinical Methods – NCBI Bookshelf
Hormonal Methods of Contraception – Women’s Health Issues – MSD Manual Consumer Version